Platelets, Coagulation and Haemostasis
Platelets, coagulation, and haemostasis are interconnected processes that stop bleeding and maintain vascular integrity. Platelets form an initial plug, coagulation stabilizes it with fibrin, and haemostasis ensures balance with anticoagulants. A key NEET and Class 11 Biology blood physiology topic.
This Story also Contains
- What are Platelets, Coagulation, and Haemostasis?
- What are Platelets?
- What is Coagulation?
- What is Haemostasis?
- Role of Anticoagulants
- Disorders of Haemostasis
- Role of Platelets and Coagulation in Health
- Platelets NEET MCQs (With Answers & Explanations)
What are Platelets, Coagulation, and Haemostasis?
Platelets, coagulation, and haemostasis represent sequential events involved in the physiological process, which assures that upon injury, excessive bleeding does not occur. It follows, therefore, that in appreciation of the processes involved in maintaining the integrity of the vasculature and the response of the body to trauma, knowledge of these concepts is required.
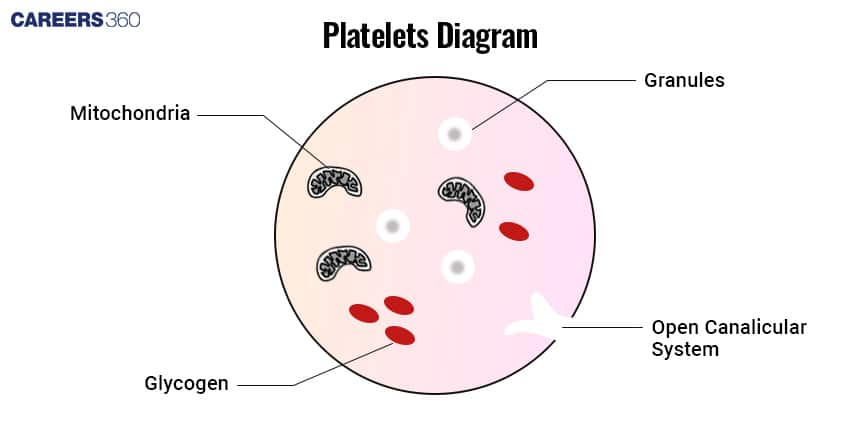
What are Platelets?
Platelets are very small, typically 2-4 micrometres in diameter, disc-shaped fragments of cells whose origin is from the megakaryocytes in the bone marrow. Platelets contain numerous granules that store clotting factors, growth factors, enzymes, and other molecules operative for their functions.
In haemostasis, they form a temporary plug at the site of vascular injury. The injury in blood vessels activates the platelets. This includes changes in shape, adhesion, and aggregation.
What is Coagulation?
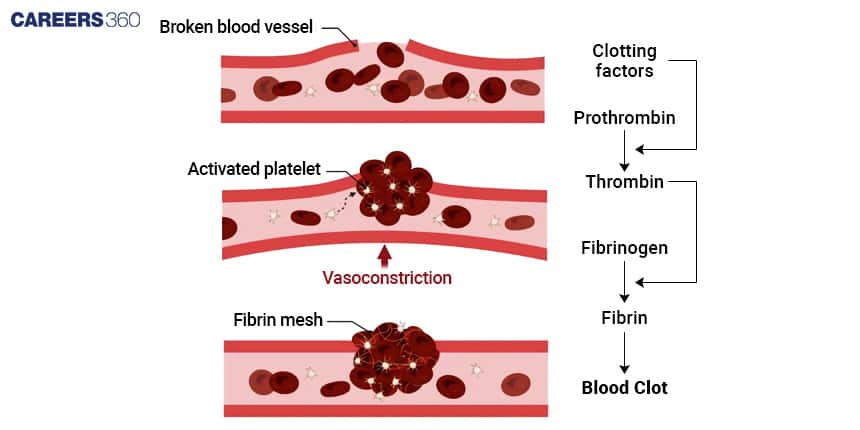
Coagulation is the complex series of biochemical reactions finally leading to the formation of a stable blood clot. It involves a variety of clotting factors, most of which are proteins synthesized in the liver.
Intrinsic Pathways
The intrinsic pathway of blood clotting is more complex than the extrinsic pathway, and it occurs slowly, usually requiring several minutes. The intrinsic pathway is so named because its activators are contained within (intrinsic to) the blood, outside tissue damage is not needed.
Extrinsic Pathways
The extrinsic pathway of blood clotting has fewer steps than the intrinsic pathway and occurs rapidly, within seconds if trauma is severe. It is so named because a tissue protein leaks into the blood from cells outside (extrinsic to) blood vessels and initiates the formation of prothrombinase.
Role of Clotting Factors
Clotting factors are proteins involved in the coagulation cascade. They are denoted by Roman numerals, for example, Factor I, and Factor II, and act to form a fibrin mesh around the platelet plug, thus stabilizing it.
The clotting factors activate in an orderly sequence. Thus, the effect is a cascade that amplifies the response and results in the very rapid formation of a clot.
What is Haemostasis?
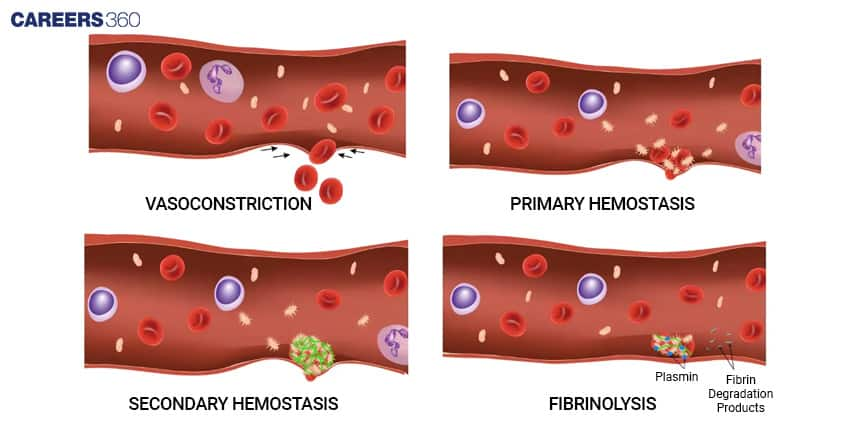
Haemostasis is a physiological process that stops bleeding and prevents its occurrence, therefore maintaining the integrity of the circulatory system after a vascular injury.
There are three main steps: vascular spasm, platelet plug formation, and coagulation.
Vascular Spasm
When blood vessels are damaged, the smooth muscle in their walls contracts immediately, a reaction called vascular spasm. This reduces blood loss for several minutes to several hours. The spasm is probably caused by damage to the smooth muscle, by substances released from activated platelets, and by reflexes initiated by pain receptors.
Platelet Plug Formation
The activated platelets start adhering to the exposed collagen fibres in the site of injury, thereby forming a plug temporarily. The platelets release some chemical signals which attract more and more platelets into the site to aggregate and form a larger plug.
Coagulation And Fibrin Formation
Due to the coagulation cascade, usually soluble plasma protein fibrinogen is converted to insoluble protein which weaves a mesh to replace the platelet plug.
Stabilization of Clot
Once a clot is formed, it plugs the ruptured area of the blood vessel and thus stops blood loss. Clot retraction is the tightening of the fibrin clot. As the clot retracts, it pulls the edges of the damaged vessel closer together, decreasing the risk of further damage.
Role of Anticoagulants
Anticoagulants are factors which prevent coagulation and halt excessive clotting. This balances the haemostatic system.
Natural Anticoagulants
Natural anticoagulants are substances present in the body that prevent unwanted blood clot formation and keep blood fluid within vessels. Examples include heparin which is released by mast cells
Clinical Anticoagulants (Heparin, Warfarin)
Clinical anticoagulants are drugs used to treat abnormal blood clot formation. The two common anticoagulants applied clinically to avoid thrombosis or excessive clotting, are heparin and warfarin.
Disorders of Haemostasis
Disorders of haemostasis are:
Hemophilia is a hereditary disorder characterized by a deficiency in one or another factor of clotting, leading to prolonged bleeding.
Thrombosis refers to the formation of a clot in the blood vessels, thereby obstructing blood flow. The serious consequences caused are a heart attack or stroke.
Role of Platelets and Coagulation in Health
Platelets and coagulation are the two most important constituents in the maintenance of blood vessel integrity, preventing excessive bleeding. These complex processes need to be understood in the diagnosis and treatment of bleeding disorders and thrombotic conditions.
Platelets NEET MCQs (With Answers & Explanations)
Types of questions that can be asked from this topic in NEET exam are:
Process of blood coagulation (Intrinsic and extrinsic pathways)
Roles of clotting factors
Formation of Platelets (thrombopoiesis)
Characteristics of Platelets (shape, count, lifespan)
Practice Questions for NEET
Q1. A decrease in platelets count is termed as
Leucocytopenia
Thrombocytopenia
Leukemia
Thrombocytic
Correct answer: 2) Thromobocytopenia
Explanation:
Thrombocytopenia is a condition where there's a decrease in the platelet count. This can lead to what are known as bleeding disorders like purpura. The normal life of a platelet is typically 5 to 9 days. When platelet count goes below 150,000 per microliter of blood, individuals might experience increased bruising and prolonged bleeding due to the impaired ability of blood to clot, which requires medical evaluation and possible treatment.
Hence, the correct answer is Option 2) Thrombocytopenia.
Q2. The blood cells involved in blood clotting are
Erythrocytes
Macrophages
Leucocytes
Thrombocytes
Correct answer: 4) Thrombocytes
Explanation:
Formed elements or blood cells constitute 45% of the blood. Blood corpuscles are of three types i.e. leukocytes (white blood cells), erythrocytes (red blood cells) and thrombocytes (blood platelets). The functions of RBC include the transport of O2 and CO2, maintenance of pH etc. The function of leukocytes in the defence against microbes and foreign particles. The function of thrombocytes is in blood clotting. The function of thrombocytes is in blood clotting.
Hence, the correct answer is option 4) Thrombocytes.
Q3. One of the common symptoms observed in people infected with Dengue fever is
Significant decrease in RBC count.
Significant decrease in WBC count.
Significant decrease in platelet count.
Significant increase in platelet count.
Correct answer: 3) Significant decrease in platelet count.
Explanation:
One frequent side effect of dengue fever, a virus spread by mosquitoes, is a low platelet count
Normal platelet count
Between 150,000 and 450,000 platelets per microliter (µL) of blood is considered normal.
Dengue platelet count
Platelet counts in dengue can fall sharply, occasionally to 10,000/µL or even less. A count below 40,000 mcL indicates a significant risk of bleeding, whereas a count below 100,000 mcL is deemed concerning.
Hence, the correct answer is option 3) Significant decrease in platelet count.
Also Read:
Frequently Asked Questions (FAQs)
The mechanisms of anticoagulant action inhibit coagulation and prevent excessive clotting for the maintenance of homeostasis within the hemostatic system.
Platelets are primarily involved in preventing haemorrhage by plugging the site of vascular injury.
Coagulation is a series of complex biochemical reactions resulting in a stable blood clot.
Vascular spasm, formation of a platelet plug, and coagulation.
This is an inherited disorder characterized by a deficiency of some clotting factors that lead to prolonged bleeding.